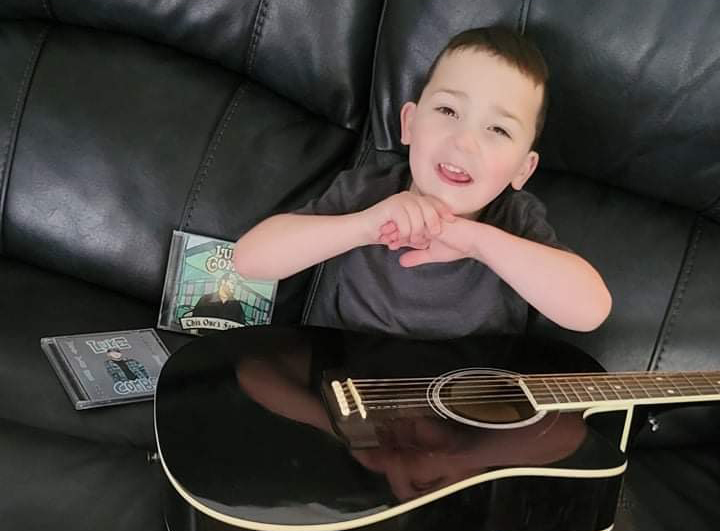
"Levi is a little comedian,"
Kristen Stanis says about her 4-year-old son, Levi. “There’s not a day that goes by that he doesn’t make me laugh. He loves music, too. Luke Combs is his favorite country artist. His grandfather got him a karaoke machine for Christmas with all the Luke Combs CDs in it. He even named his pet fish after him.”
This happy scene is not what doctors were predicting for Levi in his first year. Based on what they saw, he would never be able to sing with a karaoke machine, never tell a joke, never name a fish, never make a sound at all.
He was born with Pierre Robin syndrome, a condition marked by a deeply recessed chin and a cleft palate. To correct these problems, surgeons in another hospital (the pediatric division of an adult hospital elsewhere in Connecticut) performed jaw surgery on Levi when he was two weeks old.
Latest Articles

$1 Million Gift from Big Y Supports Connecticut Children's New Clinical Tower and Expanded Pediatric Services

A New Era of Care Begins: Connecticut Children’s Celebrates the Opening of the New Clinical Tower