Powering through a rare blood disorder
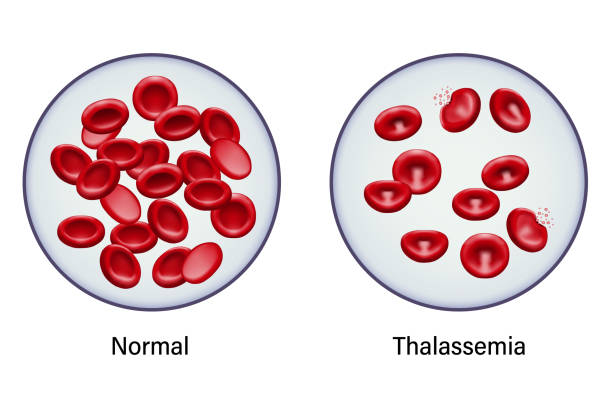
It was a call no parent wants to receive, especially at 11:30 at night. Dan and Nicole were asleep. Their four children, including 14-month-old Daniela, were sleeping. On the phone, a doctor at Connecticut Children’s was telling them, “You need to get her up and we’ll be waiting at the ER for you.” After many frustrating rounds of appointments and trips to other hospitals, the mystery of why little Daniela wasn’t growing and thriving had been solved. The results of her blood tests were back, revealing that she had beta thalassemia, a rare genetic blood disorder. Her body couldn’t make the healthy red blood cells needed to carry oxygen throughout her body.
For her parents, it was heartbreaking news. “It’s hard to learn that your child is going to be at hospitals for the rest of her life,” said Dan. Treating beta thalassemia requires regular blood transfusions. Beginning with that midnight trip to Connecticut Children’s when she was barely more than a year old, Daniela has received a blood transfusion every three weeks of her life. She admits that “it’s a little overwhelming sometimes.”
Her treatment isn’t limited to the thrice-weekly transfusions, however. She has a full team of doctors at Connecticut Children’s who oversee her care. In addition to hematologist Michael Isakoff, MD, who has treated Daniela for the past 11 years, she also receives care from endocrinology, cardiology, audiology, and ophthalmology.